Understand What Causes LC-FAOD and How It Impacts the Body
Understand What Causes LC-FAOD and How It Impacts the Body
What are long-chain fatty acid oxidation disorders (LC-FAOD)?
LC-FAOD are rare, genetic metabolic disorders that prevent the body from breaking down long-chain fatty acids into energy during metabolism.
LC-FAOD are inherited genetic conditions.
Fatty acid oxidation disorders (FAOD) are inherited conditions. For each condition, an enzyme that helps the body use fat for energy is defective.
LC-FAOD disrupt normal metabolism.
In metabolism, enzymes are needed to enable specific chemical reactions. Enzymes help the body convert fat into fatty acids and then into energy.
Metabolism is disrupted when an enzyme that helps the body use fat for energy is defective. Once glucose (sugar) is gone, the body tries to use fat without success, which disrupts energy homeostasis and leads to clinical symptoms. When the body can’t convert fat into energy as it should, levels of fatty acids build up in the heart, liver, and other organs.
LC-FAOD have recognizable signs and symptoms.
Breakdown of fatty acids is necessary for energy production when sugar, or glucose, levels are low. Without this energy supply, people with LC-FAOD may have symptoms that include, but are not limited to muscle pain, muscle weakness, low blood sugar, and fatigue.
Genetics Shape Hereditary Disorders
Hereditary metabolic disorders, including LC-FAOD, develop when children inherit defective genes that control metabolism. LC-FAOD are inherited in an autosomal recessive manner.
Autosomal recessive describes the way the genes are passed down. An autosomal recessive disorder means two copies of an abnormal gene must be present for the disease to develop.
To inherit LC-FAOD, both parents must be carriers.
Each child inherits two copies of the abnormal gene—generally one from each parent.
With each pregnancy, parents have a:
- 25% chance of having an affected child with two abnormal copies of the gene (left)
- 50% chance of having an unaffected child who is also a carrier (middle)
- 25% chance of having an unaffected child with two normal copies of the gene (right)
Metabolism Is Essential to Life
Metabolism is how the body breaks down and converts food into energy.
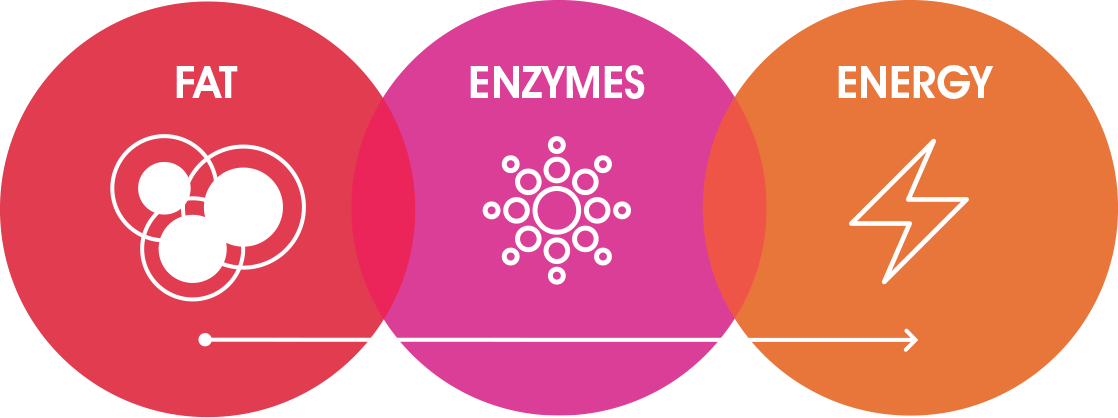
In metabolism, enzymes are needed to enable specific chemical reactions. Several specific enzymes help break down fats so that they may be turned into energy.
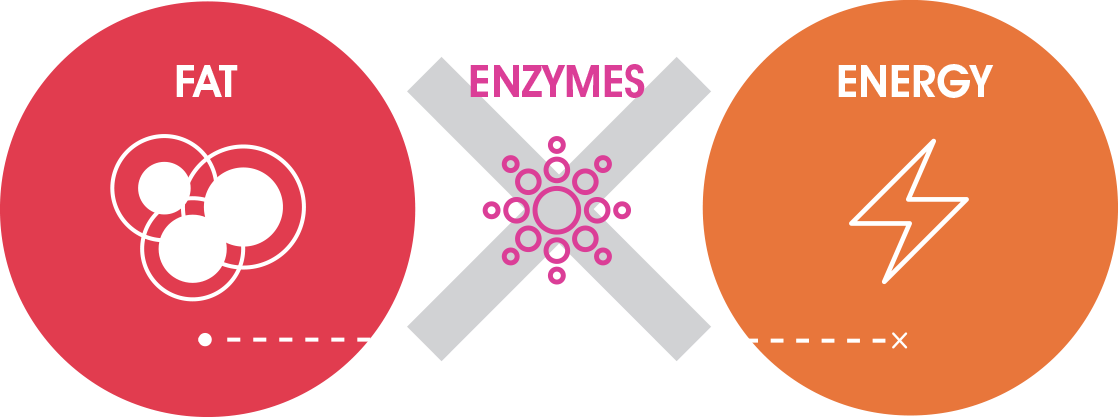
Fatty acid oxidation disorders are metabolic disorders that are caused by a lack, or defect, of the enzymes needed to break down fats.
Metabolism is disrupted when an enzyme that helps the body use stored fat for energy is missing or defective.
Once glucose (sugar) is gone, the body tries to use fat without success, which disrupts energy homeostasis and leads to clinical symptoms because of the ineffective enzyme(s) present in LC-FAOD.
How Does LC-FAOD Impact Metabolism?
Be Ready to Recognize the Signs and Symptoms
LC-FAOD are serious conditions, and people diagnosed with LC-FAOD are at risk of developing severe symptoms or health complications that can be life-threatening.
- Symptoms of LC-FAOD are episodic in nature and may lead to hospitalizations, emergency department visits, and emergency interventions.
- They can also vary within each LC-FAOD type or even between affected individuals in the same family.
- Although symptoms can appear within a few hours of birth, they may also not appear until adulthood. They can evolve over time and may differ depending on when they appear.
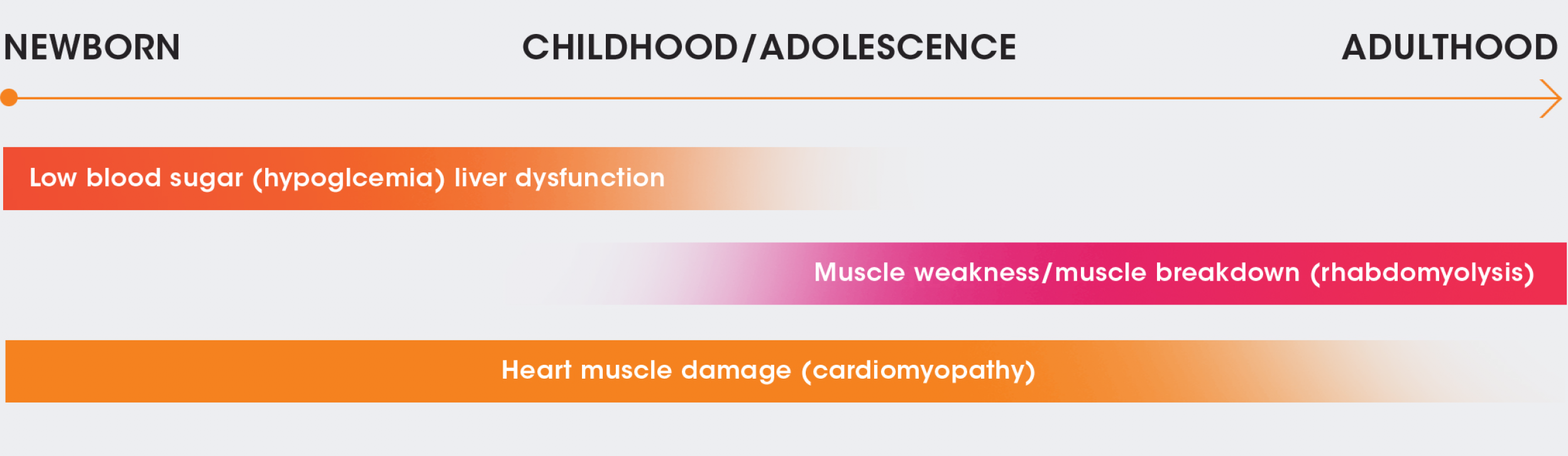
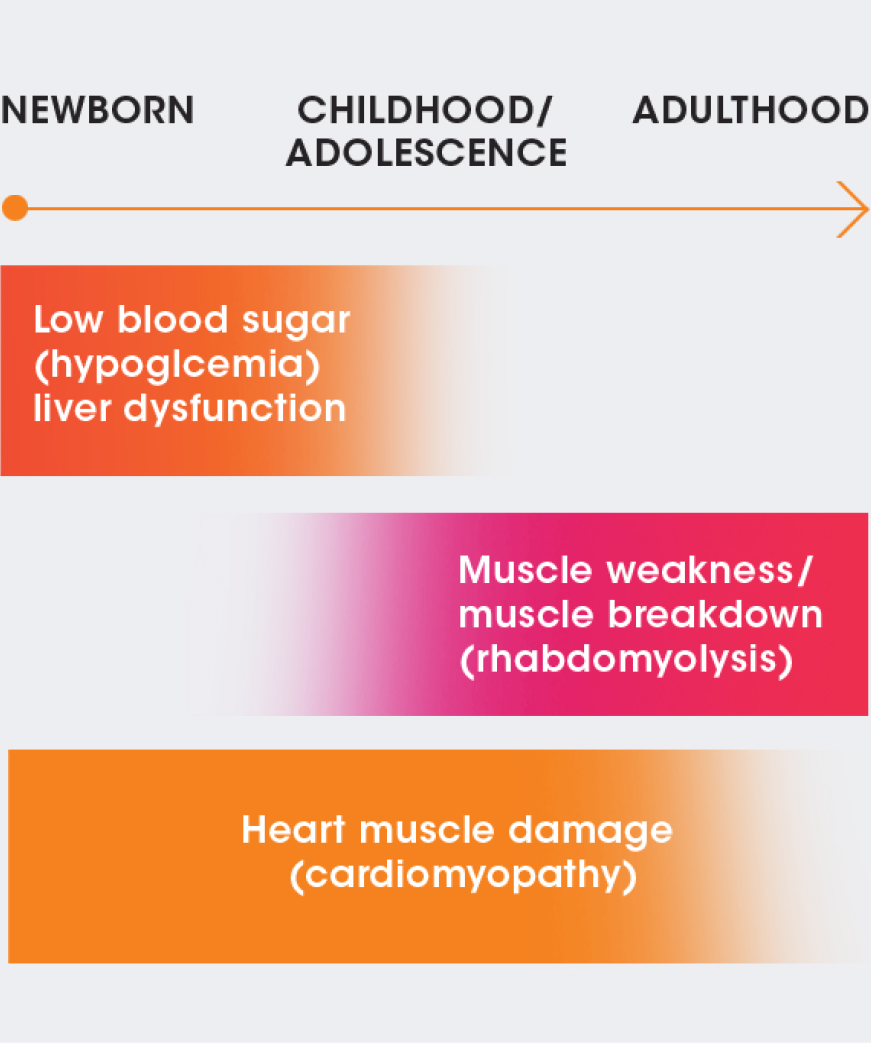
NEWBORN
CHILDHOOD/
ADOLESCENCE
ADULTHOOD
Low blood sugar (hypoglycemia)/liver dysfunction
Muscle weakness/muscle breakdown (rhabdomyolysis)
Heart muscle damage (cardiomyopathy)
Chronic Symptoms and Acute Episodes
Chronic signs and symptoms of LC-FAOD develop over time and may worsen over months to years. Chronic (persistent or recurring) symptoms may include fatigue, muscle pain, muscle cramps, muscle weakness, and foggy thinking.
They can be brought on or made worse by fasting or illness, sustained exercise, and physiologic stress and may lead to the following:
- Decreased muscle tone
(hypotonia) - Muscle pain or weakness
(myalgia or myasthenia) - Damage to the retina of eyes*
(retinopathy)
- Damage to nerves*
(peripheral neuropathy) - Liver dysfunction
(hepatic dysfunction)
*Applies to certain LC-FAOD types such as LCHAD and TFP. Consult your healthcare provider for more information.
Acute signs and symptoms of LC-FAOD develop suddenly. They usually appear during an illness or if you have skipped a meal, but they may also occur spontaneously or unpredictably.
With LC-FAOD, individuals might experience acute metabolic crises that may include serious conditions such as:
- Heart muscle damage†
(cardiomyopathy) - Muscle breakdown
(rhabdomyolysis)
- Nausea, stomach upset, appetite changes
- Low blood sugar
(hypoglycemia)
Individuals with LC-FAOD may limit their physical activity because sustained intense exercise or activity increases the risk of developing symptoms or triggering an acute episode.
†May have a chronic impact.
Issues in Infants and Young Children
Caregivers of babies and young children with LC-FAOD should watch for and be aware of symptoms of a metabolic crisis, including:
- Neurologic distress (extreme sleepiness, coma, Reye’s syndrome)
- Changes in heart beat
- Muscle weakness
- Changes in appetite or dietary requirements
Keep a record and let your healthcare team know if you experience or observe any of these signs or symptoms.
Useful Resources
Stay Informed
Sign up to receive the current disease education information in your inbox.

